Important Points:
- Overview of pelvic inflammatory disease (PID) and its impact on reproductive health.
- Common symptoms and risk factors for developing PID.
- Treatment options and preventive measures to maintain reproductive health.
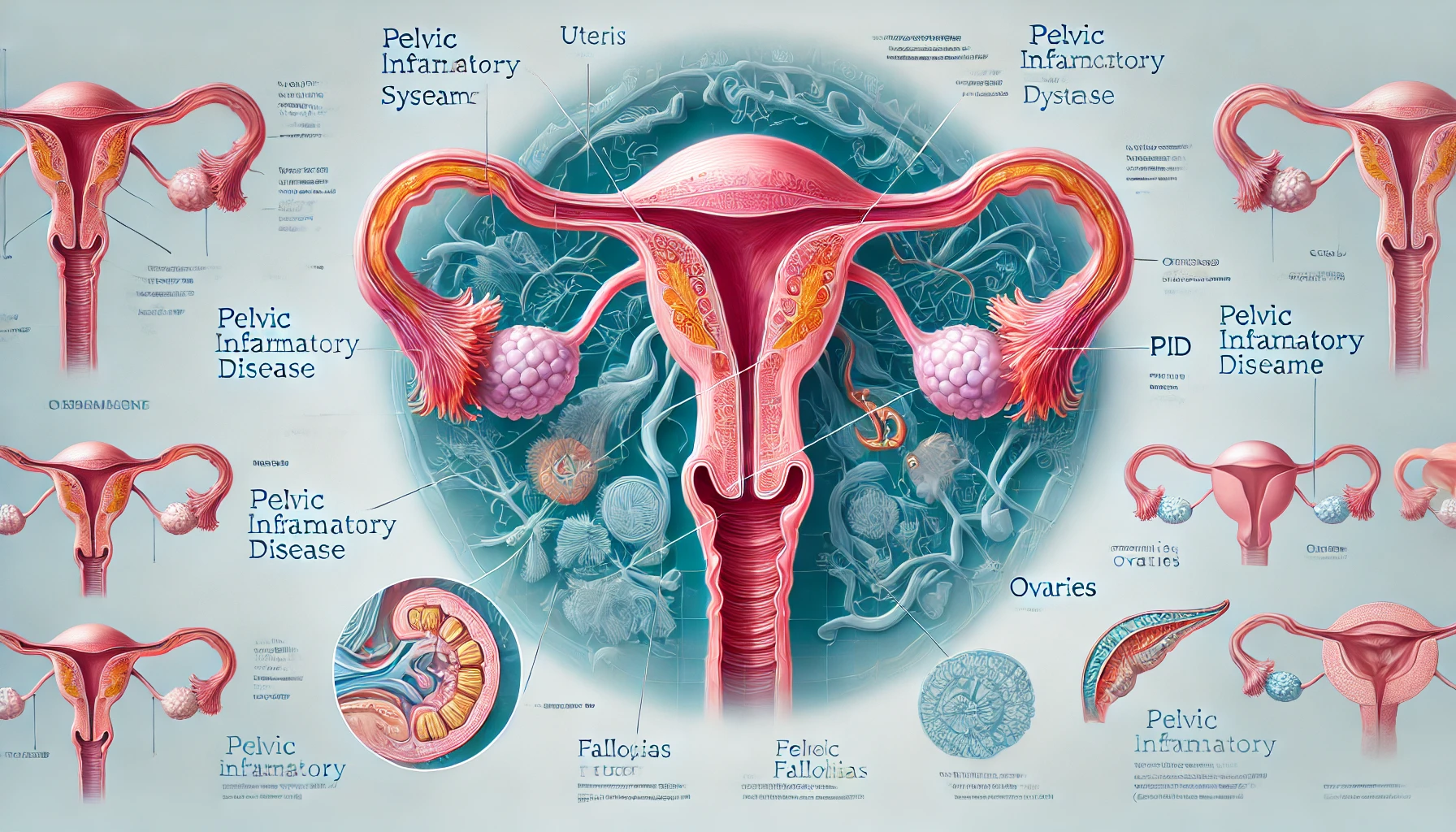
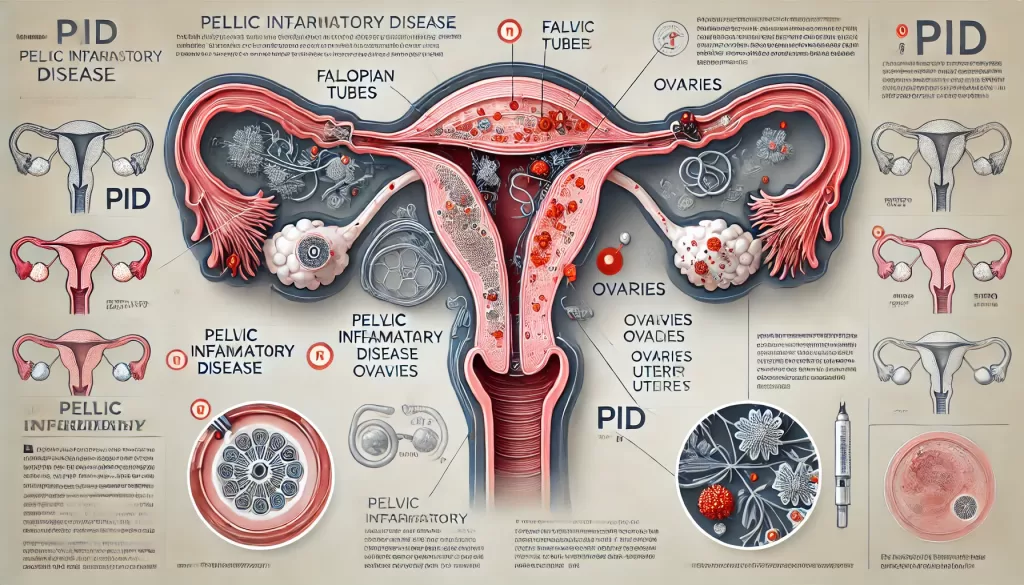
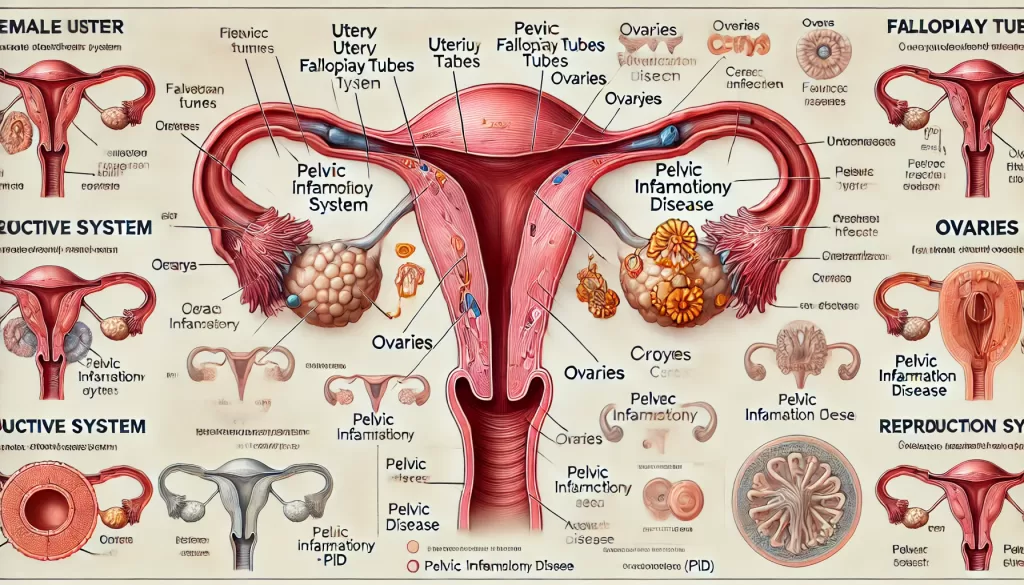
What is Pelvic Inflammatory Disease (PID)?
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs, including the uterus, fallopian tubes, and ovaries. It occurs when bacteria spread from the vagina or cervix to the upper reproductive tract. PID is a serious condition that can lead to infertility, chronic pelvic pain, and ectopic pregnancy if untreated. Early detection and treatment are crucial to prevent complications.
Symptoms of Pelvic Inflammatory Disease
Symptoms of PID can vary from mild to severe, and some women may have no symptoms at all. Common signs include:
- Pelvic or Lower Abdominal Pain: Often described as dull or cramping pain in the lower abdomen.
- Abnormal Vaginal Discharge: Yellow, green, or foul-smelling discharge is common.
- Pain During Intercourse: Discomfort or pain, especially during deep penetration.
- Irregular Menstrual Bleeding: Spotting between periods or heavier-than-normal bleeding.
- Painful Urination: A burning sensation while urinating.
- Fever and Chills: Indicate an active infection.
- Nausea or Vomiting: May occur in severe cases.
Pelvic Inflammatory Disease
What Causes PID?
PID is typically caused by bacteria, most commonly:
- Sexually Transmitted Infections (STIs): Chlamydia trachomatis and Neisseria gonorrhoeae are the primary culprits.
- Normal Vaginal Bacteria: If these bacteria enter the upper reproductive tract, they can cause infection.
- Post-Surgical Infections: Procedures such as childbirth, abortion, or IUD insertion can increase risk.
Risk Factors for PID
Certain factors increase the likelihood of developing PID:
- Unprotected Sex: Having multiple sexual partners or not using condoms increases risk.
- Previous History of PID: Increases susceptibility to recurrent infections.
- Young Age: Women under 25 are at higher risk due to an immature cervix.
- Douching: Can disrupt the natural balance of bacteria in the vagina, facilitating infection.
- STI History: A history of chlamydia or gonorrhea significantly raises the risk.
How is PID Diagnosed?
Diagnosis involves a combination of medical history, physical exams, and tests:
- Pelvic Exam: Checks for tenderness, swelling, or abnormal discharge.
- Swabs and Cultures: Tests vaginal and cervical samples for bacterial infections.
- Blood and Urine Tests: Identify signs of infection or inflammation.
- Ultrasound: Detects abnormalities in the reproductive organs.
- Laparoscopy: A minimally invasive procedure to examine the pelvic area directly.
Pelvic Inflammatory Disease
Complications of PID
Untreated PID can lead to serious complications, including:
- Infertility: Scarring of the fallopian tubes can block egg movement.
- Ectopic Pregnancy: Scarring increases the risk of a fertilized egg implanting outside the uterus.
- Chronic Pelvic Pain: Persistent pain due to scarring or inflammation.
- Abscess Formation: Pockets of infected fluid may form in the reproductive organs.
Treatment Options for Pelvic Inflammatory Disease
Prompt treatment is essential to prevent long-term complications. Options include:
1. Antibiotics
- A combination of broad-spectrum antibiotics is typically prescribed to address the most common bacteria.
- Oral or Intravenous Treatment: Depending on severity, antibiotics may be taken orally or administered intravenously.
2. Hospitalization
- Severe cases or those involving abscesses may require hospitalization for intensive treatment.
3. Surgery
- Rarely needed but may be required to drain abscesses or remove scar tissue.
Preventing Pelvic Inflammatory Disease
Taking steps to reduce your risk of PID is essential for reproductive health:
- Practice Safe Sex: Use condoms and maintain a monogamous relationship.
- Get Regular STI Screenings: Early detection of chlamydia or gonorrhea can prevent the spread of infection.
- Avoid Douching: It disrupts the natural vaginal flora, increasing infection risk.
- Follow Post-Surgical Instructions: Adhere to guidelines after gynecological procedures to prevent infection.
Living with PID
For women recovering from PID, lifestyle adjustments can promote healing and prevent recurrence:
- Complete All Medications: Even if symptoms improve, finish your prescribed antibiotics.
- Avoid Sexual Activity: Refrain from intercourse until the infection has completely cleared.
- Monitor Symptoms: Report any persistent pain, fever, or abnormal discharge to your doctor.

Pelvic Inflammatory Disease
When to See a Doctor
Seek immediate medical attention if you experience:
- Severe pelvic or abdominal pain.
- High fever with nausea or vomiting.
- Persistent abnormal discharge or bleeding.
Early diagnosis and treatment of PID are crucial to prevent complications and protect reproductive health.
Conclusion
Pelvic inflammatory disease is a serious condition that requires prompt attention to prevent long-term reproductive health issues. By recognizing the symptoms, seeking timely treatment, and adopting preventive measures, women can reduce their risk of PID and maintain overall well-being. Regular medical check-ups and safe practices are essential for protecting reproductive health.