Important Points:
- What dyspnea is and how it affects the body
- Common causes of dyspnea, including respiratory and heart-related issues
- How dyspnea is diagnosed and managed
- Treatment options and lifestyle adjustments to improve breathing
Understanding Dyspnea and How to Manage Shortness of Breath
What is Dyspnea?
Dyspnea, commonly known as shortness of breath, is a sensation of difficulty or discomfort in breathing. This can range from mild discomfort to an intense feeling of breathlessness. Dyspnea can occur suddenly or develop gradually over time and may be a temporary response to exertion, stress, or altitude. However, it can also signal underlying medical conditions related to the heart, lungs, or other bodily systems. Understanding the causes and treatments for dyspnea can help those affected manage symptoms and improve their quality of life.
Symptoms of Dyspnea
- Labored Breathing
- How It Feels: Individuals with dyspnea often feel as if they’re working harder to inhale or exhale. Breathing may feel shallow or more rapid than usual.
- When It Happens: This can occur during physical exertion, while lying down, or even at rest in more severe cases.
- Chest Tightness
- How It Feels: Dyspnea is often accompanied by a sensation of tightness or pressure in the chest, which can intensify the feeling of breathlessness.
- When It Happens: Chest tightness may come and go or remain constant, depending on the underlying cause.
- Wheezing or Noisy Breathing
- How It Sounds: Wheezing, a whistling sound during breathing, may occur alongside dyspnea, especially in cases related to asthma or respiratory infections.
- When It Happens: Wheezing is often worse during exertion or when lying down, and it can indicate airway constriction.
- Increased Heart Rate
- How It Feels: Dyspnea can cause a racing or pounding heart, which may be a response to the body’s increased oxygen demand.
- When It Happens: An elevated heart rate is common when dyspnea is caused by physical activity, stress, or heart-related conditions.
- Cyanosis (Bluish Tint to Skin or Lips)
- How It Looks: In severe cases, a bluish tint to the skin or lips may occur due to low oxygen levels in the blood.
- When It Happens: Cyanosis is a serious symptom that requires immediate medical attention, as it indicates a significant oxygen deficiency.
Common Causes of Dyspnea
- Respiratory Conditions
- Asthma: Asthma causes inflammation and narrowing of the airways, leading to episodes of wheezing, tightness, and shortness of breath.
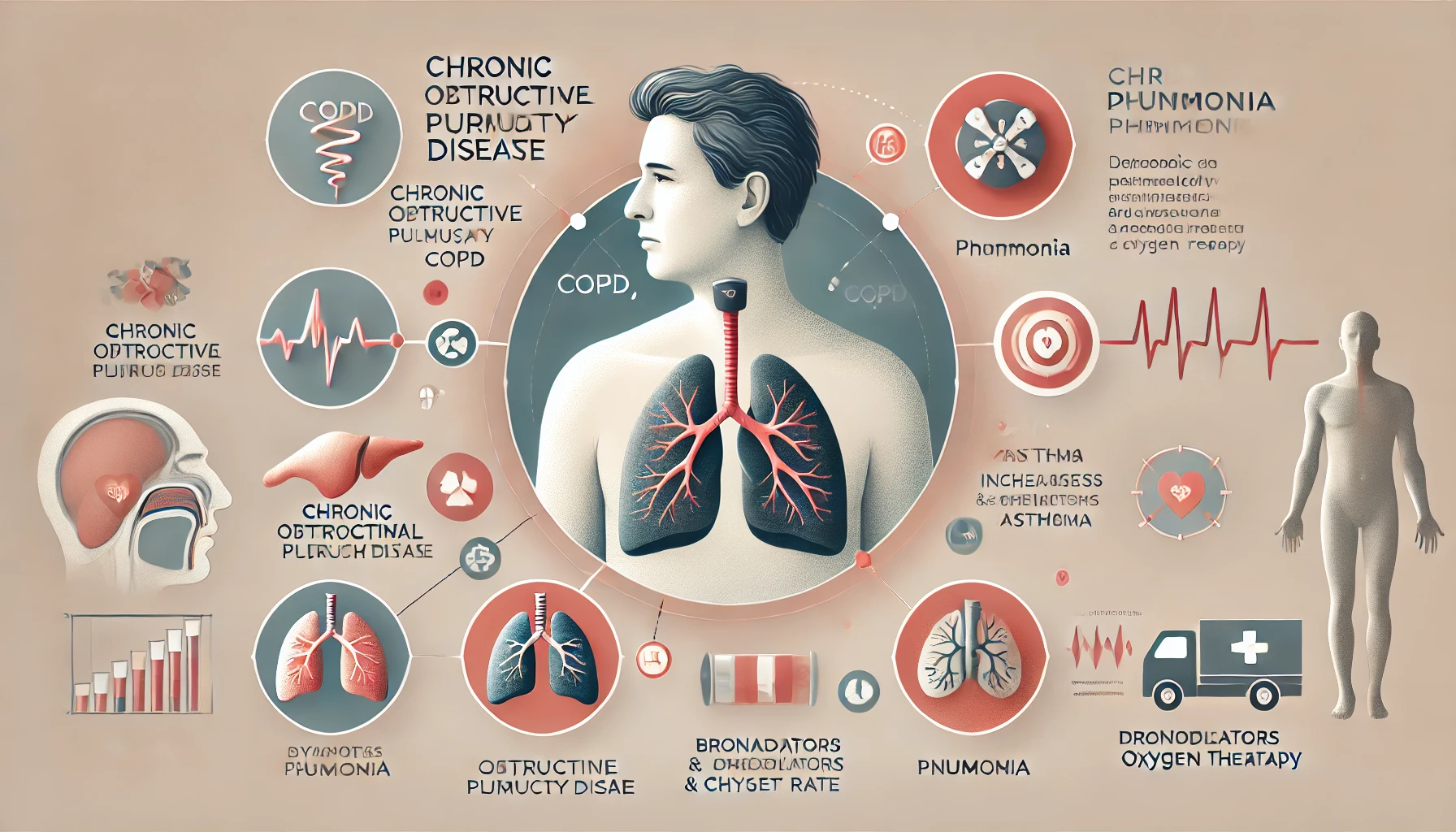
- Chronic Obstructive Pulmonary Disease (COPD): COPD includes conditions like emphysema and chronic bronchitis, which damage the lungs and make breathing difficult.
- Pneumonia: Pneumonia is a lung infection that can cause inflammation and fluid buildup, leading to shortness of breath.
- Pulmonary Embolism: A pulmonary embolism is a blood clot in the lung that can obstruct blood flow and cause severe dyspnea.
- Heart Conditions
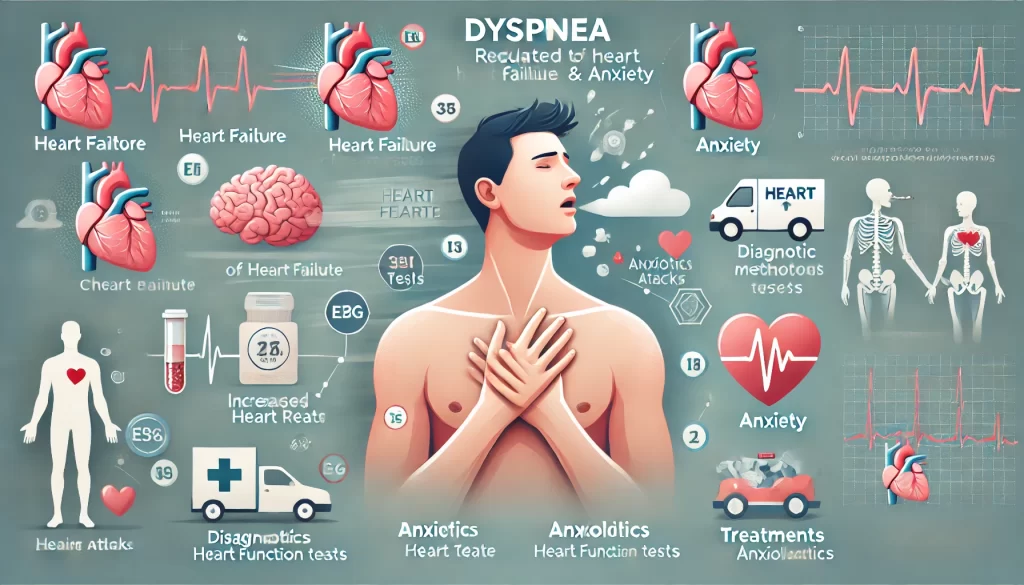
- Heart Failure: Heart failure reduces the heart’s ability to pump blood effectively, leading to fluid buildup in the lungs and shortness of breath.
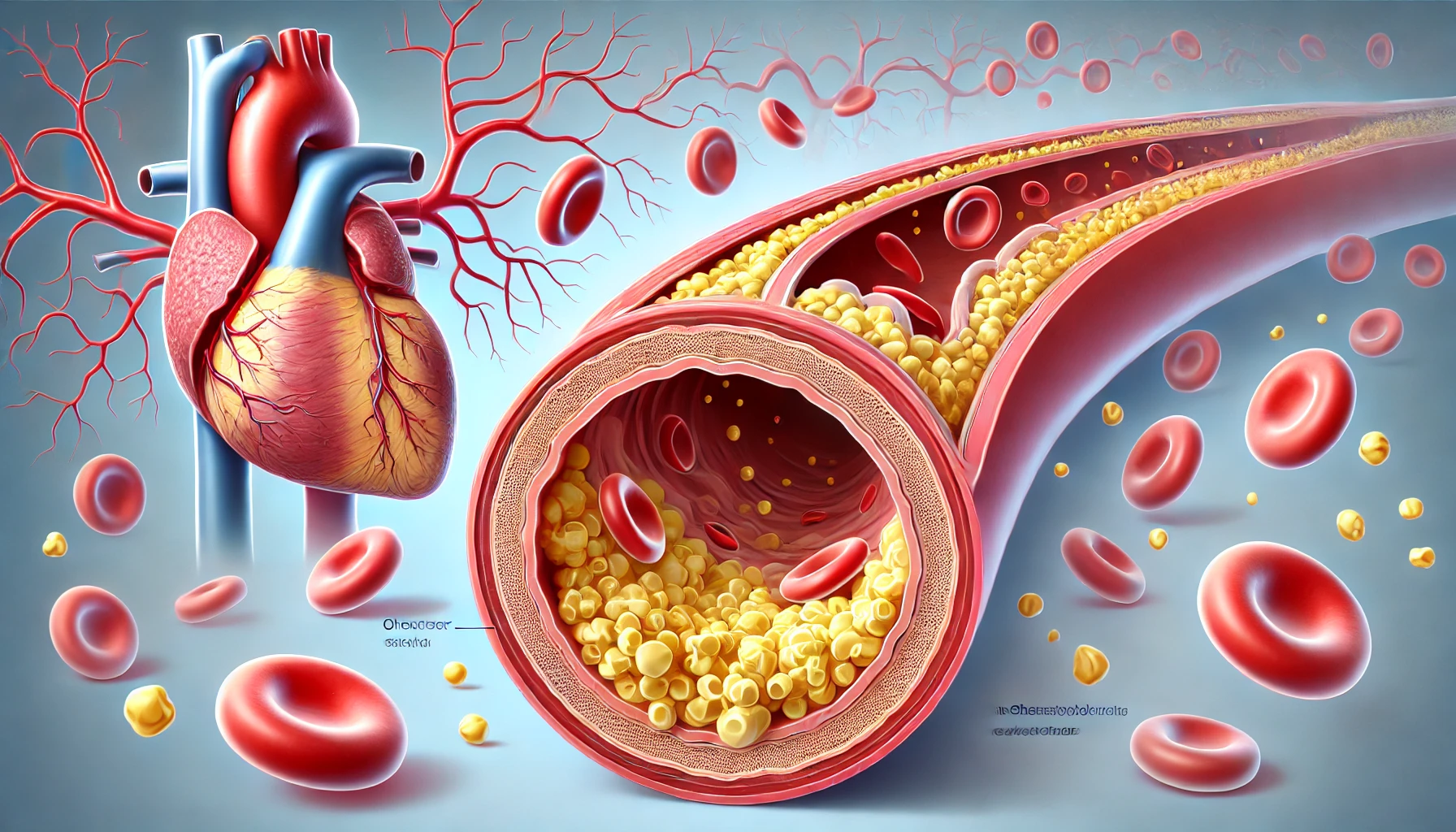
- Coronary Artery Disease (CAD): CAD causes reduced blood flow to the heart, which can trigger chest pain and breathlessness, especially during physical activity.
- Arrhythmias: Abnormal heart rhythms can impact blood flow, causing symptoms like dyspnea and palpitations.
- Anxiety and Panic Disorders
- How It Causes Dyspnea: Anxiety and panic attacks can lead to hyperventilation (rapid breathing), creating a sensation of shortness of breath. This can be mistaken for a physical problem but is often rooted in emotional distress.
- When It Happens: Dyspnea caused by anxiety may occur suddenly and be accompanied by symptoms like a racing heart, sweating, and dizziness.
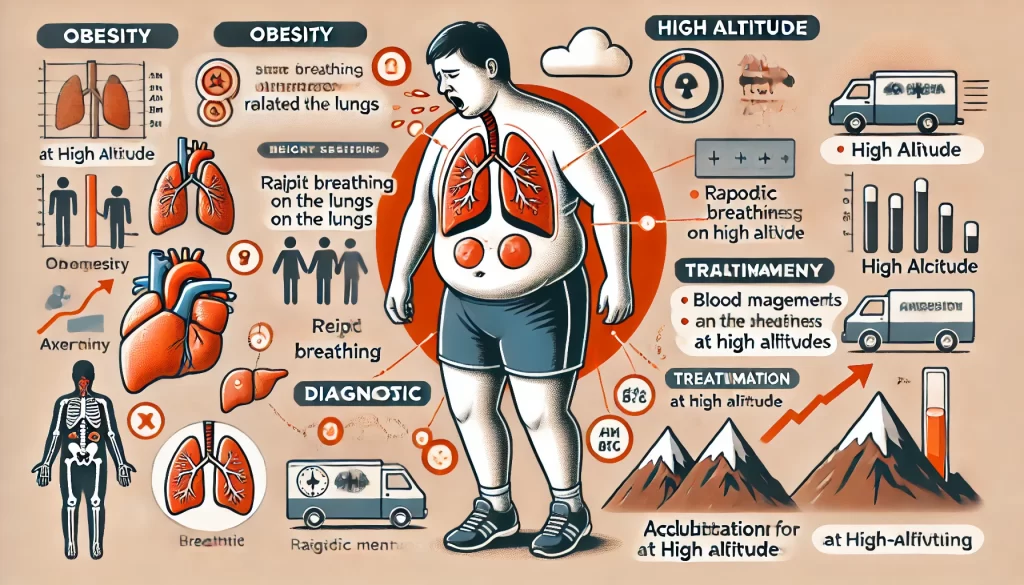
- Other Contributing Factors
- Obesity: Excess weight can put strain on the lungs and diaphragm, making breathing more difficult, especially during physical exertion.
- Anemia: Low red blood cell count reduces oxygen transport in the blood, leading to feelings of breathlessness.
- High Altitude: At high altitudes, oxygen levels are lower, causing breathlessness even in healthy individuals as the body adjusts to the reduced oxygen.
Diagnosing Dyspnea
Diagnosing the cause of dyspnea involves a series of tests and evaluations:
- Medical History and Physical Exam
- What It Involves: A doctor will ask about the duration, severity, and circumstances of your breathlessness, as well as any other symptoms or health conditions.
- Why It’s Important: This helps identify whether dyspnea is due to respiratory, cardiac, or other underlying issues.
- Imaging Tests (Chest X-ray or CT Scan)
- What It Shows: Imaging can reveal abnormalities in the lungs or heart, such as fluid buildup, infections, or structural changes.
- When It’s Used: Imaging tests are often ordered if respiratory or cardiac causes are suspected.
- Lung Function Tests (Spirometry)
- What It Measures: Spirometry assesses lung capacity and airflow, which can help diagnose conditions like asthma and COPD.
- When It’s Used: Lung function tests are often used when chronic respiratory issues are suspected.
- Blood Tests
- What It Checks For: Blood tests can detect anemia, infection, or signs of other underlying health issues that might contribute to dyspnea.
- Electrocardiogram (ECG) and Echocardiogram
- What It Shows: ECG and echocardiogram evaluate heart function, checking for abnormalities in rhythm, structure, and blood flow.
- When It’s Used: These tests are commonly ordered if heart disease or heart failure is suspected as a cause of dyspnea.
Treatment Options for Dyspnea
- Medications
- Bronchodilators: Medications that open the airways, commonly prescribed for asthma and COPD, can relieve shortness of breath.
- Diuretics: For heart failure patients, diuretics help remove excess fluid from the body, reducing lung congestion and improving breathing.
- Anxiolytics: For anxiety-related dyspnea, medications that reduce anxiety may alleviate symptoms of shortness of breath.
- Oxygen Therapy
- When It’s Used: Oxygen therapy is prescribed for those with chronic respiratory conditions, such as COPD, or heart failure patients with low oxygen levels.
- How It Helps: Supplemental oxygen helps improve blood oxygen levels, making breathing easier and reducing strain on the heart and lungs.
- Pulmonary Rehabilitation
- What It Involves: Pulmonary rehabilitation combines education, exercise, and breathing techniques to improve lung function and build endurance.
- Who Benefits: This program is particularly helpful for individuals with COPD or other chronic lung conditions.
- Lifestyle Adjustments
- Exercise and Weight Management: Regular, moderate exercise can improve cardiovascular and respiratory endurance. Weight management reduces strain on the lungs and heart.
- Diet and Hydration: A balanced diet and adequate hydration support overall health and may improve symptoms of dyspnea, especially in cases related to anemia or obesity.
When to Seek Emergency Help for Dyspnea
Seek emergency care if you experience:
- Severe shortness of breath that worsens rapidly
- Chest pain, especially if it radiates to your arm, neck, or jaw
- Cyanosis (bluish tint to skin or lips), indicating low oxygen levels
- Sudden onset of dyspnea following an injury or accident
- Difficulty speaking or breathing normally
Conclusion: Managing Dyspnea for a Better Quality of Life
Dyspnea can be caused by various health conditions, from respiratory and cardiac issues to anxiety. Understanding the root cause and managing symptoms through medication, lifestyle changes, and therapy can significantly improve quality of life. If you experience persistent or worsening shortness of breath, seek medical attention to identify the underlying cause and receive appropriate treatment. With the right approach, you can find relief and enjoy improved respiratory health.





 Next Post
Next Post